No, you don’t.
In medicine, certainty is a very dangerous thing. It’s ok to be certain about things like the price of gas or your dislike of prunes (couldn’t blame you).
Certainty in medicine is quite another.
And, although politically incorrect to say it, I’m finding a frustrating amount of unjustified certainty among the ranks of the “mini-docs”. By mini-doctors, I mean all the permutations of lesser-trained white coat-donners. The PA’s, ARNP’s, Dr. RN’s, LPN’s, etc.

Exposed to about 1/3 of the training of the average primary care M.D. (if that), these sorta-doctors function in American medicine with nearly complete autonomy (and are constantly pushing for more).
I have no problem with these relatively new additions to the medical field. I myself criticized my training as too long, redundant and costly while enduring it.
But the more I work with patients who see them, the more I run into decision-making that is flat-out problematic.
I should mention that many P.A.’s I’ve trained with were clearly smarter than me. A couple of the ARNP’s I currently work with are easily as bright or brighter than my – shall we say – earth-friendly mental wattage.
But I’ve learned that smart brains often don’t lead to good medicine. In my opinion, what makes the best medical decision-maker is an acute awareness of ignorance.
You could call it intellectual humility, if you wish. It could be that all the hours of training in medicine really just cultivates this humility to refinement. I can see the value of that.
In the last week, I have dealt with numerous decisions of certainty in medicine that were completely unjustified. All were made by PA’s and ARNP’s. As patients described their experiences, I could tell their previous providers were of the para-doc variety even before they confirmed it for me.
“I’m here for antibiotics, Dr. Secretwave101.”
“Really? What for?”
“I have pneumonia again. I had it 5 times last year. I just have to come in and get antibiotics for it. It’s such a pain!”
“PNEUMONIA? FIVE times in a year? Are you sure? Confirmed by chest X-ray? Do you know the organism? Bacterial each time? Which lung? Was it a particular lobe? Were you hospitalized? Did you have pulmonary scarring as a child?”
“Uhhh. I don’t know any of that stuff. I just need the medicine. I always just come in with this cough and get the medicine.”
Pneumonia is a big freaking deal. Real pneumonia kills people. Like, healthy, not-old, not-sick people. Real pneumonia almost never hits someone 5 times in a year. Once, and you’ve had a tough previous 12 months. You get it 5 times and you’re basically telling me that you’ve spent the previous year in a hospital with chest tubes, IV meals and a bag to catch your pee.
There were two problems with the patient encounter. One, the patient wasn’t well educated by her provider, who clearly had numerous opportunities to clarify things for her over the previous year. She didn’t have pneumonia 5 times, she had a cough.
The provider also never worked up the cough to see what it actually was. No X-rays. No sputum cultures. No pulmonary function tests. Just antibiotics. Broad-spectrum antibiotics.
 In another post, I will describe why throwing antibiotics toward a cough with no evidence of bacterial involvement is absolutely catastrophic for the long-term survival of the human species. That statement is a rare instance on this blog where I’m not stating hyperbole, either.
In another post, I will describe why throwing antibiotics toward a cough with no evidence of bacterial involvement is absolutely catastrophic for the long-term survival of the human species. That statement is a rare instance on this blog where I’m not stating hyperbole, either.
Antibiotic resistance is real, and the results of it will kill you.
I also recently recommended that my sister-in-law take her son into an urgent care center to be evaluated for what sounded like strep throat. That would be, Streptococcus Group A pharyngitis.
“Did you know,” I asked her, “why we treat strep throat?”
“Well, he could get really sick, right?”
“Yes, but not from the throat infection.”
“So, we’re not treating the throat?”
“No. That goes away. Most pharyngitis is viral and goes away. Even bacterial goes away. We only need to treat one specific cause of pharyngitis, Group A Strep, because it can also cause heart disease, kidney disease and all kinds of other stuff.”
“I didn’t know that.” She replied.
I didn’t either. Not until years into my training.
The next day, I found that my nephew was taken to a P.A. at the local Urgent Care and without a culture or any other objective work up, he is diagnosed with “strep throat” and given antibiotics.
“I don’t even need to test this, the symptoms are so classic.” The “doctor” reportedly said.
Two days later, the boy’s little sister gets sick. There’s no culture from the back of brother’s throat. We have no idea if what he had was viral, bacterial, fungal or nothing at all. He may not have even needed the antibiotics, and likely didn’t have the right ones if he did need them.
Now we have no idea what his sister has. Is it the same thing? Is it something new? I guess we’ll just throw some antibiotic at her, too and say they both had STREP THROAT, even though we have no evidence of this.

Certainty in medicine flat-out leads to bad medical care. Everybody has the urge to think they’ve got this or that totally nailed from time to time. Doctors too. Maybe doctors more than other health professionals.
But my experience so far is that certainty increases with less training.
My warning to you is this: If your health care provider is CERTAIN about your health problems, you don’t have a very good doctor. Humility comes from a wide differential diagnosis.
In nature, the humble survive; the proud die.

Wow. I remember a post (months ago) you put somewhere on the internet, either SDN, WSJ or some blog and you were basically rolling over to say a mid-level was pretty much the same. Glad to see the change, but sad it has to be true.
LikeLike
I once pointed out that mid-levels look the same as primary care docs from the perspective of accountants and businessmen.
I don’t remember rolling over on the topic. Ugh!
LikeLike
To be fair, doctors have been known to do this as well as mid-levels. I think the difference is that if a doctor has a natural or previously developed bent towards trouble-shooting or intellectual curiosity, MD/DO training is more likely to foster it.
LikeLike
I think in general if anyone says they “know for sure,” one should be skeptic. This is where the patients need to be a more conscious consumer. A person needs to take responsibility for their health and the approaches used to treat their health. If you walk into a doctor’s office with total blind faith that whoever you see knows how to fix you, you’re in for problems. The “white coat” syndrome takes into affect.
It doesn’t matter who you are, you have to use your brain and take responsibility for yourself. In this day and age with so much information out there, if a doctor says you have pneumonia you should probably be reading up on that. Not just doing the easy thing, the convenient thing by getting some pills to fix it.
LikeLike
As the mom of the nephew in the story above, I have to defend myself by saying that I DID ask the LNP to do the rapid strep anway, and she basically blew me off. I do try to be educated – and when I am unsure, or get unsatisfying care, I call the Dr in the family to get real information. 🙂
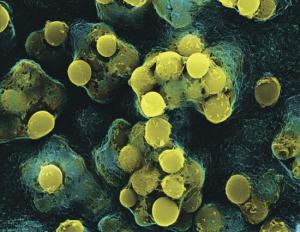
Oh, and I’m pretty sure my son’s throat didn’t look like that…I checked it the day before we went in to the Dr and it definitely looked red, but nothing like that.
LikeLike
Niffer – Making you feel like you need to defend yourself for following the advice of a paid medical professional is the last thing I would want from this post.
This critique is reserved only for intellectually-lazy health care providers who, by virtue of their professional standing, can adversely influence even the most diligent recipients of health care.
LikeLike
I am more than willing to let my doctor enjoy her well-earned humility and overfunded uncertainty, so long as we can agree to bill my visits according to a “global” problem price list — that is, so long as I don’t end up subsidizing the process of her second-guessing herself.
I know that you are proposing common sensical things — cultures, basic imaging, etc. — but how far out into complexity do you take this? Are you going to be more on the lookout for zebras than horses?
LikeLike
Really, an excellent question. And my answer is no, hopefully I won’t be over-looking (expensively) for zebras when the obvious problem is in plain sight.
That said, pretending to have knowledge is disingenuous and can be dangerous.
Doctors can’t know everything, but higher-level thinking coupled with (usually) a few simple tests provides much better care than uncritical, knee-jerk diagnoses made in ignorance.
LikeLike
How very odd! I left “here,” went yonder, to Dr. Rob’s blog, where I read this:
“Here’s another mystery: If I order a rapid strep test that comes back positive, I can’t say the strep test was done for the diagnosis of Strep Throat (ICD-034.0) or it won’t get paid for. If, however, I use the diagnosis of Pharyngitis (ICD-462) it is paid for. The ‘logic’ of this is that if you know the patient has strep, why would you do a strep test? This makes no sense, because the only way we can make the diagnosis in our office is to do the test. This ‘logic’ holds for EKG’s, and Lab work done in the office. You cannot use the test results to justify the test itself.”
What message about diagnostics is the financial system in medicine trying to instill in youse doctors what want to be sagely humble and hardly all-knowing?
LikeLike
In my opinion, Dr. Rob is off base on this one, and the insurance companies have it right (first and last time you’ll probably EVER hear me saying that).
It makes no sense to order a test for a condition someone already has. In the case of strep throat, it is presumptuous to say the person has it without a culture. Therefore, there’s no sense in billing for that diagnosis until you have the test to support the diagnosis. What IS certain, is that the patient has pharyngitis – that is, inflammation of the pharynx. This diagnosis can be made visually. The CAUSE of the pharyngitis is almost always microscopic…hence the need for a test.
LikeLike